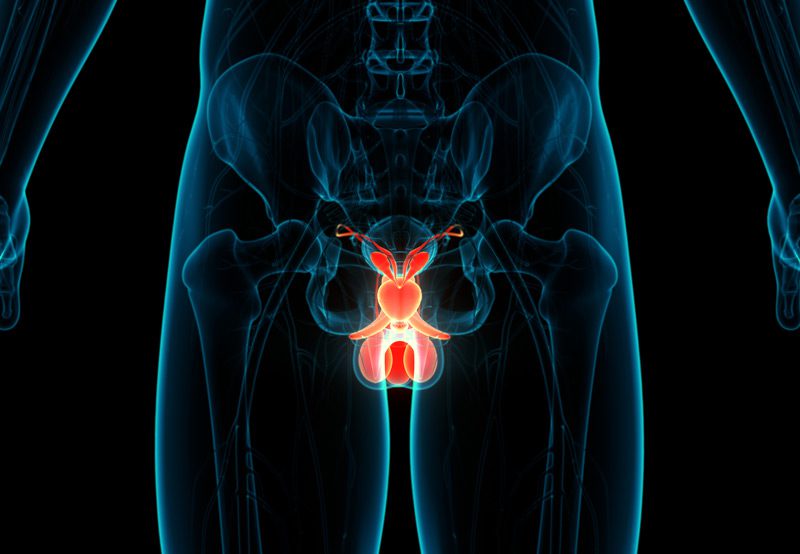
Male genital reconstruction refers to a range of surgical procedures used to restore the form and function of the penis, scrotum, and surrounding structures. These procedures are often necessary following trauma, cancer treatment, infections, congenital abnormalities, or complications from previous surgeries. The goal is to improve urinary, sexual, and psychological well-being through functional and aesthetic restoration.
Why Male Genital Reconstruction Is Performed
Reconstructive surgery may be indicated for:
- Traumatic Injuries: Including those from accidents, burns, or penetrating trauma affecting the penis, scrotum, or urethra.
- Infections and Complications: Such as Fournier’s gangrene, a life-threatening soft tissue infection that can result in extensive tissue loss.
- Congenital Conditions: Including hypospadias, epispadias, or buried penis, where normal genital development is disrupted.
- Cancer Surgery Aftermath: Reconstruction may follow partial or total penectomy (penile cancer) or scrotectomy.
- Lymphedema and Scrotal Swelling: Long-standing swelling may necessitate excision and reconstruction.
- Severe Peyronie’s Disease or Erectile Dysfunction: When curvature or scarring severely impacts sexual function, reconstruction may be needed.

Common Procedures in Male Genital Reconstruction
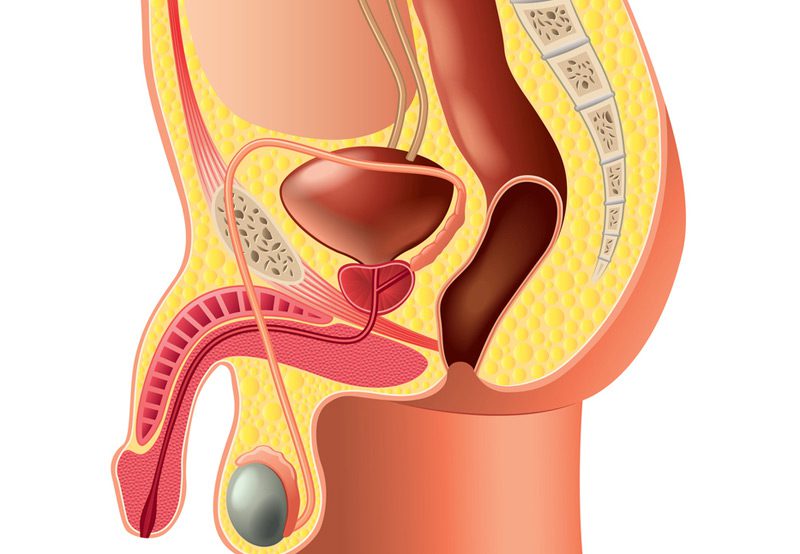
- Penile Reconstruction: This can include realignment, skin grafts, or full phalloplasty in complex cases. Reconstructive options depend on how much tissue remains and the goals of the patient.
- Scrotoplasty: Reconstruction or reshaping of the scrotum, often using local tissue or flaps. This may follow trauma, infection, or cancer surgery.
- Urethral Reconstruction (Urethroplasty): Restores urinary function when the urethra is damaged or strictured.
- Buried Penis Repair: Involves releasing hidden penile tissue and reconstructing surrounding skin, often in obese patients or after childhood trauma.
- Skin Grafting and Flap Surgery: Used to replace tissue lost to infection, burns, or surgical excision. Grafts may be taken from the thigh, groin, or other donor sites.
- Testicular Prosthesis Placement: In cases of testicular loss or removal, prosthetic implants restore scrotal appearance and symmetry.
Recovery and Outcomes
Most procedures are performed under general anesthesia. Recovery depends on the complexity of the reconstruction and whether multiple stages are required. Pain, swelling, and temporary catheterization are common in the early postoperative period. Long-term outcomes generally show improved self-image, sexual confidence, and urinary function.
Is Genital Reconstruction Right for You?
If you’ve experienced genital trauma, disfigurement, or functional issues, reconstruction may be an option. A urologist or reconstructive surgeon will assess your condition and recommend a personalized treatment plan that addresses both form and function.
