
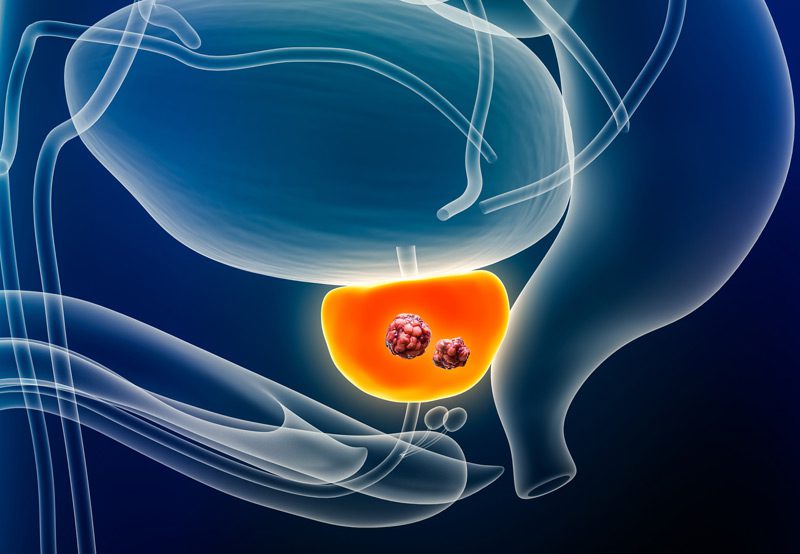
While prostate cancer treatments are often effective in managing or eliminating cancer, they can be associated with short-term and long-term complications. The specific risks vary depending on the type of treatment used: whether surgery, radiation therapy, hormone therapy, or active surveillance. Understanding potential complications helps patients make informed decisions and prepare for the road to recovery.
Surgical Complications (Radical Prostatectomy)
Surgical removal of the prostate (radical prostatectomy) is a common treatment for localized prostate cancer. While generally safe, it carries risks, including:
- Urinary Incontinence: Difficulty controlling urine flow is common initially after surgery and may persist long-term in some cases.
- Erectile Dysfunction: Damage to nerves involved in erection may occur, especially in non–nerve-sparing procedures.
- Bleeding or Infection: Like all major surgeries, there is a risk of bleeding, infection, or complications from anesthesia.
- Bladder Neck Contracture: Scar tissue can form at the junction where the bladder connects to the urethra, narrowing the passage and affecting urine flow.
- Lymphedema: Swelling in the legs or groin may result if lymph nodes are removed during surgery.

Radiation Therapy Complications
External beam radiation or brachytherapy can effectively treat prostate cancer but may also impact surrounding tissues:
- Urinary Symptoms: Radiation cystitis may cause burning with urination, urgency, or frequency.
- Rectal Irritation: Radiation proctitis may lead to rectal bleeding, discomfort, or bowel habit changes.
- Erectile Dysfunction: Nerve and vascular damage can occur gradually after radiation therapy.
- Fatigue: Radiation treatment may cause temporary or ongoing fatigue during and after treatment.
Hormone Therapy (Androgen Deprivation Therapy) Complications
Hormone therapy lowers testosterone levels to slow cancer growth, but this systemic change can lead to multiple side effects:
- Hot flashes and night sweats
- Loss of libido and erectile dysfunction
- Fatigue and mood changes
- Weight gain and muscle loss
- Bone thinning (osteoporosis)
- Increased risk of metabolic syndrome or cardiovascular issues
Managing Side Effects
Many complications can be addressed with medical or lifestyle interventions:
- Pelvic Floor Therapy: Helps manage urinary incontinence.
- Medications or Devices: Aid in erectile function recovery.
- Diet and Exercise: Help mitigate hormone therapy side effects.
- Supportive Care: Mental health support, physical therapy, and urologic follow-up improve quality of life.
Close communication with your care team ensures that complications are managed early and appropriately.
